Clinical Trials for 12 Years or Older
TRIAL 1 (STRIVE): Patients with CF age 12 years and older with a G551D mutation. KALYDECO® (ivacaftor) achieved significant improvements across multiple clinical endpoints in patients with a G551D mutation1-3
ON THIS PAGE: Study Design | Summary of Results
Mutation Eligible for Study1 (mutation in bold was enrolled)
G551D
STUDY DESIGN1
- Trial 1 was a 48-week, Phase 3, randomized, double-blind, placebo-controlled trial (N=161) in patients with CF age 12 years and older (mean age: 26 years) and a G551D mutation
- Patients had to have FEV1 40%-90% predicted at screening [mean FEV1 64% predicted at baseline (range: 32%-98%)]
- Patients received KALYDECO 150 mg or placebo every 12 hours with fat-containing food, in addition to their prescribed CF therapies. Use of hypertonic saline was not permitted
Primary endpoint1: Improvement in lung function as determined by the mean absolute change from baseline in ppFEV1 through 24 weeks
Other efficacy endpoints3: Absolute change in ppFEV1 through Week 48, improvement from baseline in CFQ-R Respiratory Domain score through Weeks 24 and 48, time to first pulmonary exacerbation through Weeks 24 and 48, absolute change from baseline in body weight at Weeks 24 and 48, and absolute change from baseline in sweat chloride concentration through Weeks 24 and 48
SUMMARY OF RESULTS1,3,4
Significant improvements in lung function were seen through 24 weeks and persisted through 48 weeks1,3,4
Treatment difference through:
24 weeks (primary endpoint)a
+10.6 points
(95% CI: 8.6, 12.6; P<0.0001)
48 weeks (other endpoint)a
+10.5 points
(95% CI: 8.5, 12.5; P<0.0001)
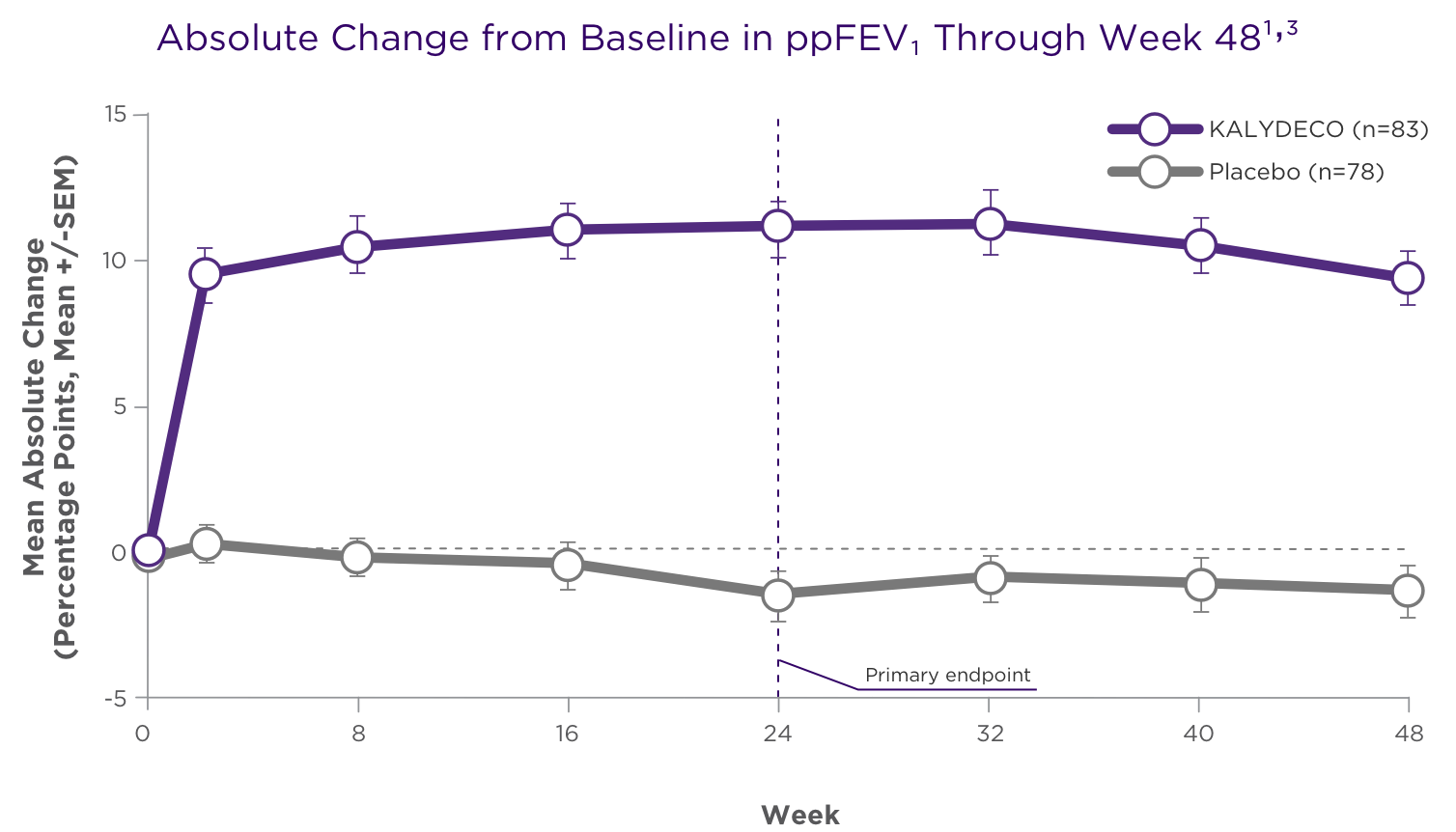
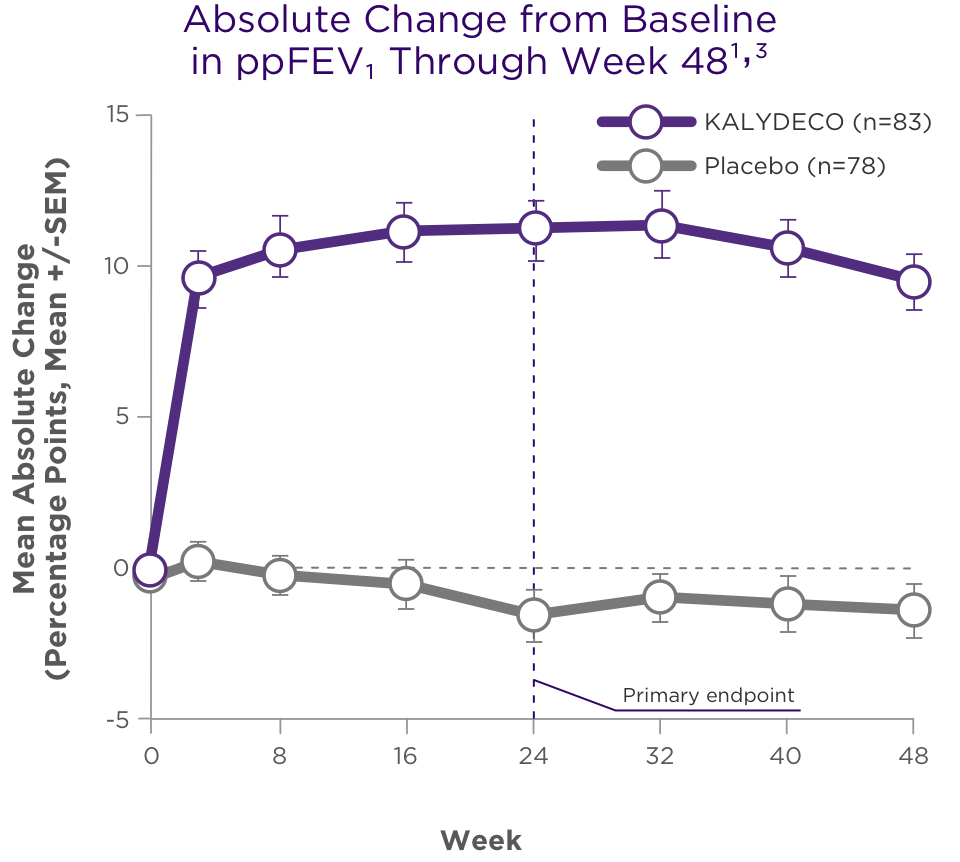
aTreatment difference = effect of KALYDECO – effect of placebo.1
Primary endpoint was assessed through 24 weeks for Trial 1 and was based on a mixed-effects model for repeated measures (MMRM).1,3
Clinical endpoints studied in Trial 1 for KALYDECO showed significant, sustained improvements vs placebo1
CFQ-R RESPIRATORY DOMAIN SCORE
Treatment difference through:
24 weeksa
+8.1 points
(95% CI: 4.7, 11.4; P<0.0001)
48 weeksa
+8.6 points
(95% CI: 5.3, 11.9; P<0.0001)
RELATIVE RISK OF PULMONARY EXACERBATION
Treatment difference through:
24 weeksa
60% reduction
(HR, 0.40; P=0.0016)
48 weeksa
54% reduction
(HR, 0.46; P=0.0012)
- Pulmonary exacerbation was defined as a change in antibiotic therapy (IV, inhaled, or oral) as a result of 4 or more of 12 pre-specified sino-pulmonary signs/symptoms1
BODY WEIGHT
Treatment difference at:
24 weeksa
+2.8 kg
(95% CI: 1.8, 3.7; P<0.0001)
48 weeksa
+2.7 kg
(95% CI: 1.3, 4.1; P=0.0001)
- Changes in BMI normalized for age and sex in patients <20 years of age were consistent with absolute change from baseline in weight1
SWEAT CHLORIDE
Treatment difference through:
24 weeksa
−48 mmol/L
(95% CI: -51, -45; P<0.0001)
48 weeksa
−48 mmol/L
(95% CI: -51, -45; P<0.0001)
- There was no direct correlation between decrease in sweat chloride levels and improvement in lung function (FEV1)1
aTreatment difference = effect of KALYDECO – effect of placebo.1
HR, hazard ratio; IV, intravenous; BMI, body mass index.
TRIAL 7: Patients with CF age 12 years and older with specific ivacaftor-responsive mutations. KALYDECO® (ivacaftor) improved lung function vs placebo overall and across all pre-specified subgroups1
ON THIS PAGE: Study Design | Summary of Results
Mutations Eligible for Study1,2 (mutations in bold were enrolled)
- Patients were heterozygous for the F508del mutation and a second mutation predicted to be responsive to ivacaftor
- The 5 splice mutations studied were: 2789+5G→A, 3272-26A→G, 3849+10kbC→T, 711+3A→G, E831X (n=94 for KALYDECO and n=97 for placebo)
- The 11 missense mutations studied were: A455E, D1152H, D579G, L206W, P67L, R1070W, R117C, R347H, R352Q, S945L, S977F (n=62 for KALYDECO and n=63 for placebo)
- D110E, D110H, D1270N, E56K, E193K, F1052V, F1074L, K1060T, R74W
STUDY DESIGN1,3
CFTR-targeted therapy expanded to patients with responsive splice and missense mutations1
- Trial 7 was an 8-week, randomized, double-blind, placebo-controlled, 2-period, crossover design trial (N=246) in patients with CF age 12 years and older (mean age: 35 years)a
- Patients had to have FEV1 40%-90% predicted at screening [mean FEV1 62% predicted at baseline (range: 35%-94%)]
- Patients received KALYDECO 150 mg or placebo every 12 hours with fat-containing food, in addition to their prescribed CF therapies1,3
Primary endpoint1: Mean absolute change from baseline in ppFEV1 to the average of Weeks 4 and 8
Key secondary endpoint1: Absolute change from baseline in CFQ-R Respiratory Domain score averaged at Weeks 4 and 8
SUMMARY OF RESULTS1,4
Significant improvement in ppFEV1 by Day 15 maintained through 8 weeks1,4
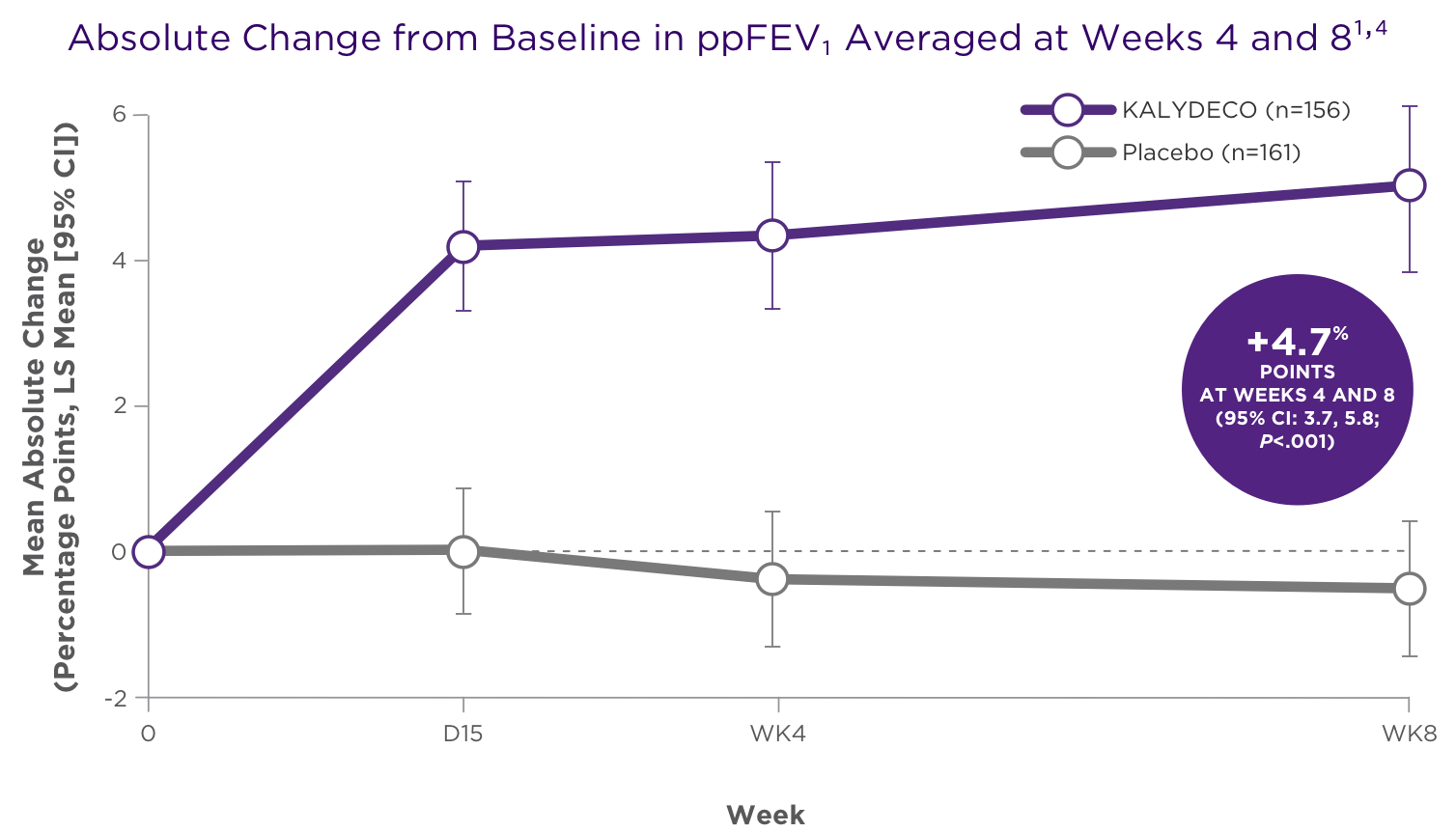
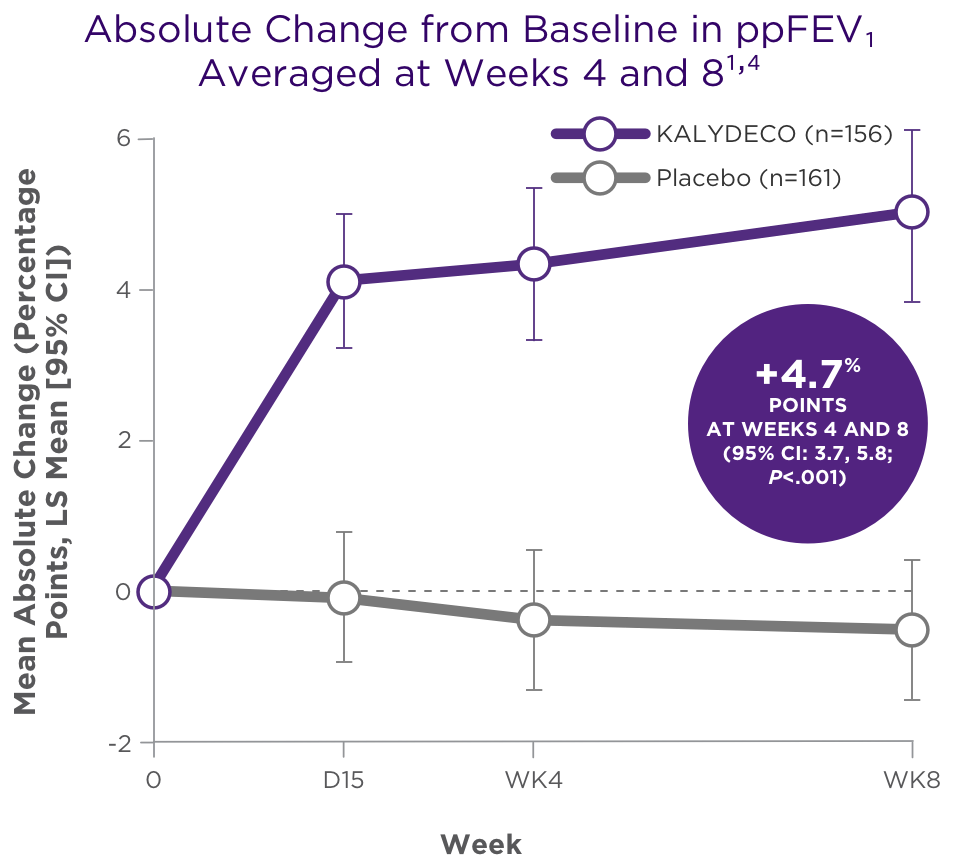
Adapted with permission from Rowe SM et al. N Engl J Med. 2017;377(21);2024-2035.
aThe complete study design and results are not reported here; only the KALYDECO and placebo groups are shown
Significant improvement in CFQ-R Respiratory Domain score from baseline for KALYDECO vs placebo overall1,4
- The overall treatment difference was 9.7 points (95% CI: 7.2, 12.2; P<0.0001)
- For individual mutations, results varied by genotype and ranged from -8.3 to 44.4; see full Prescribing Information for results by mutation. These were ad hoc analyses
IMPORTANT SAFETY INFORMATION
WARNINGS AND PRECAUTIONS
Transaminase (ALT or AST) Elevations
- Elevated transaminases have been reported in patients with CF receiving KALYDECO. Transaminase elevations were more common in patients with a history of transaminase elevations or in patients who had abnormal transaminases at baseline. ALT and AST should be assessed prior to initiating KALYDECO, every 3 months during the first year of treatment, and annually thereafter. For patients with a history of transaminase elevations, consider more frequent monitoring of liver function tests
- Patients who develop increased transaminase levels should be closely monitored until the abnormalities resolve. Dosing should be interrupted in patients with ALT or AST of greater than 5 times the upper limit of normal (ULN). Following resolution of transaminase elevations, consider the benefits and risks of resuming KALYDECO
INDICATIONS AND USAGE
KALYDECO is indicated for the treatment of cystic fibrosis (CF) in patients age 1 month and older who have at least one mutation in the CFTR gene that is responsive to ivacaftor potentiation based on clinical and/or in vitro assay data.
If the patient's genotype is unknown, an FDA-cleared CF mutation test should be used to detect the presence of a CFTR mutation followed by verification with bi-directional sequencing when recommended by the mutation test instructions for use.
INDICATIONS AND USAGE
KALYDECO is indicated for the treatment of cystic fibrosis (CF) in patients age 1 month and older who have at least one mutation in the CFTR gene that is responsive to ivacaftor potentiation based on clinical and/or in vitro assay data.
If the patient's genotype is unknown, an FDA-cleared CF mutation test should be used to detect the presence of a CFTR mutation followed by verification with bi-directional sequencing when recommended by the mutation test instructions for use.
IMPORTANT SAFETY INFORMATION
WARNINGS AND PRECAUTIONS
Transaminase (ALT or AST) Elevations
- Elevated transaminases have been reported in patients with CF receiving KALYDECO. Transaminase elevations were more common in patients with a history of transaminase elevations or in patients who had abnormal transaminases at baseline. ALT and AST should be assessed prior to initiating KALYDECO, every 3 months during the first year of treatment, and annually thereafter. For patients with a history of transaminase elevations, consider more frequent monitoring of liver function tests
- Patients who develop increased transaminase levels should be closely monitored until the abnormalities resolve. Dosing should be interrupted in patients with ALT or AST of greater than 5 times the upper limit of normal (ULN). Following resolution of transaminase elevations, consider the benefits and risks of resuming KALYDECO
Hypersensitivity Reactions, Including Anaphylaxis
- Hypersensitivity reactions, including cases of anaphylaxis, have been reported in the postmarketing setting. If signs or symptoms of serious hypersensitivity reactions develop during treatment, discontinue KALYDECO and institute appropriate therapy. Consider the benefits and risks for the individual patient to determine whether to resume treatment with KALYDECO
Concomitant Use With CYP3A Inducers
- Use of KALYDECO with strong CYP3A inducers, such as rifampin, substantially decreases the exposure of ivacaftor, which may reduce the therapeutic effectiveness of KALYDECO. Co-administration of KALYDECO with strong CYP3A inducers, such as rifampin, rifabutin, phenobarbital, carbamazepine, phenytoin, and St. John's wort is not recommended
Cataracts
- Cases of non-congenital lens opacities/cataracts have been reported in pediatric patients treated with KALYDECO. Baseline and follow-up ophthalmological examinations are recommended in pediatric patients initiating treatment with KALYDECO
ADVERSE REACTIONS
Serious Adverse Reactions
- Serious adverse reactions, whether considered drug-related or not by the investigators, which occurred more frequently in patients treated with KALYDECO included abdominal pain, increased hepatic enzymes, and hypoglycemia
Most Common Adverse Reactions
- The most common adverse reactions in the 221 patients treated with KALYDECO were headache (17%), upper respiratory tract infection (16%), nasal congestion (16%), nausea (10%), rash (10%), rhinitis (6%), dizziness (5%), arthralgia (5%), and bacteria in sputum (5%)
- The safety profile for the CF patients enrolled in clinical trials (Trials 3-8) was similar to that observed in the 48-week, placebo-controlled trials (Trials 1 and 2)
USE IN SPECIFIC POPULATIONS
Pediatric Use
- The safety and effectiveness of KALYDECO in patients with CF younger than 1 month of age have not been established. The use of KALYDECO in children under the age of 1 month is not recommended
- Use of KALYDECO in patients aged 1 to less than 6 months born at a gestational age less than 37 weeks has not been evaluated
Click here to access full Prescribing Information.
References:
1. KALYDECO [prescribing information]. Boston, MA: Vertex Pharmaceuticals Incorporated; August 2023. 2. US National Library of Medicine. ClinicalTrials.gov. Available at https://clinicaltrials.gov/ct2/show/NCT00909532. Accessed May 1, 2023. 3. Ramsey BW, Davies J, McElvaney NG, et al. A CFTR potentiator in patients with cystic fibrosis and the G551D mutation. N Engl J Med. 2011;365(18):1663-1672. 4. Ramsey BW, Davies J, McElvaney NG, et al. A CFTR potentiator in patients with cystic fibrosis and the G551D mutation. N Engl J Med. 2011;365(18)(suppl):1663-1672.

